Our Summary
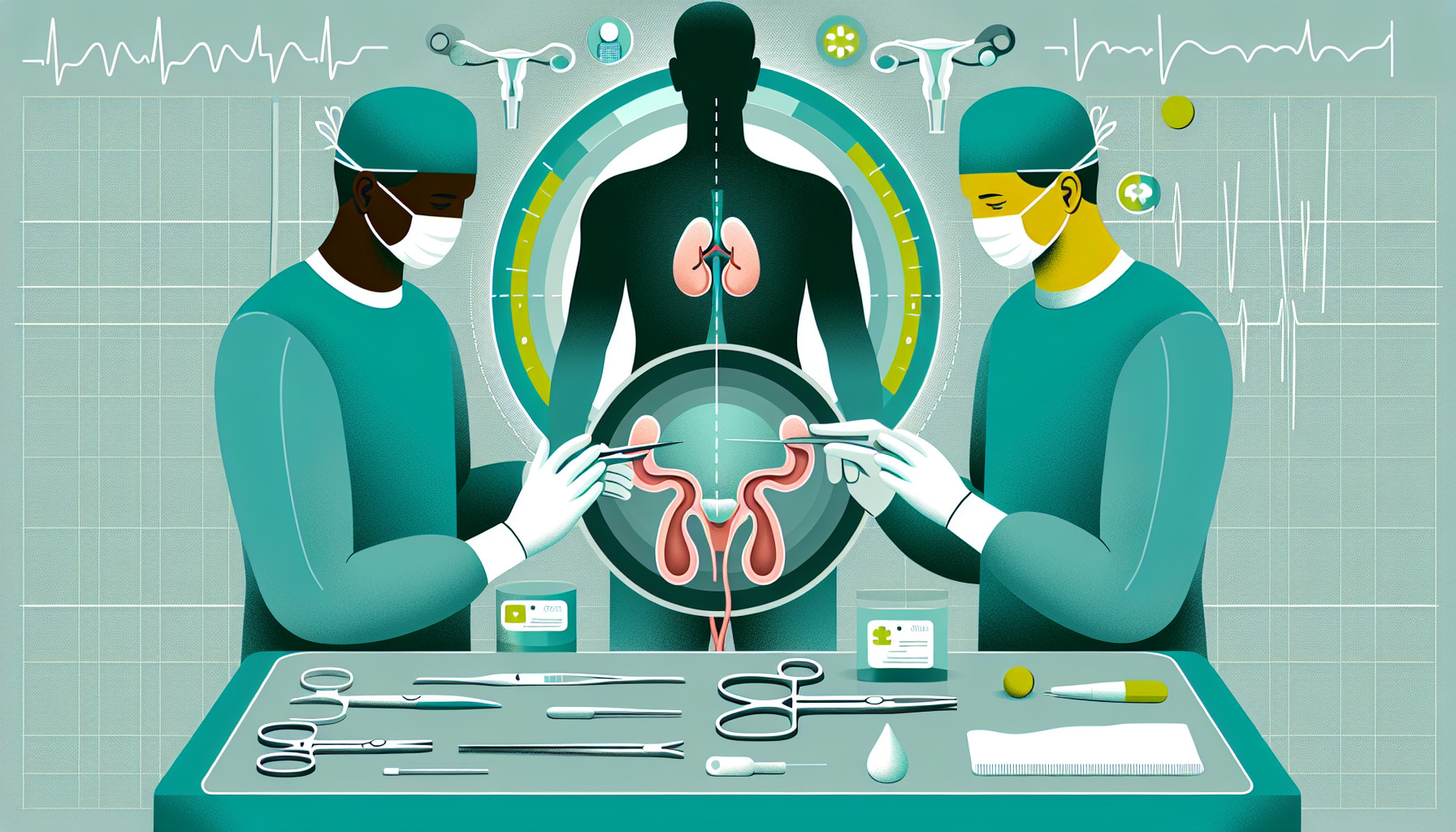
This research paper discusses the treatment of a type of bladder cancer that affects the muscle and is localized (not spread to other parts of the body). This type represents approximately 20% of all new bladder cancer cases. Patients with this cancer have two main treatment options: removal of the bladder (radical cystectomy) or radiation therapy. However, both these treatments can significantly affect the patient’s quality of life. They can impact the patient’s ability to function independently, their urinary and sexual activities, social and emotional health, body perception, and can cause significant psychological stress. The paper also points out that, compared to other cancers such as breast or prostate cancer, there isn’t enough high-quality research exploring the effects of bladder cancer treatments on patients’ quality of life.
FAQs
- What is a cystectomy and how is it related to bladder cancer treatment?
- What are the potential impacts of bladder cancer treatments like cystectomy on a patient’s quality of life?
- How does the research on bladder cancer treatment’s effects on quality of life compare to other cancers such as breast or prostate cancer?
Doctor’s Tip
A doctor might advise a patient undergoing cystectomy to discuss potential side effects, such as changes in urinary and sexual function, with their healthcare team and to seek support from a counselor or support group to help cope with any emotional or psychological challenges that may arise during treatment and recovery. It is also important for the patient to follow their healthcare team’s recommendations for post-operative care and rehabilitation to optimize their recovery and overall well-being.
Suitable For
Patients who are typically recommended cystectomy are those with muscle-invasive bladder cancer that has not responded to other treatments such as radiation or chemotherapy. Additionally, patients with high-grade non-muscle invasive bladder cancer or recurrent bladder cancer may also be candidates for cystectomy. It is important for patients to discuss their treatment options with their healthcare provider to determine the best course of action for their specific situation.
Timeline
Before cystectomy:
- Patient is diagnosed with muscle invasive bladder cancer
- Patient undergoes various tests and imaging to determine extent of cancer
- Patient discusses treatment options with healthcare team, including cystectomy
- Patient may undergo neoadjuvant chemotherapy before surgery
- Patient may have a pre-operative appointment to discuss surgery and recovery process
- Patient may need to make lifestyle changes or prepare for surgery, such as quitting smoking or adjusting medications
After cystectomy:
- Patient undergoes surgery to remove the bladder and create a urinary diversion (ileal conduit or neobladder)
- Patient stays in the hospital for several days to recover
- Patient may experience pain, fatigue, and discomfort post-surgery
- Patient may require physical therapy or rehabilitation to regain strength and mobility
- Patient may need to adjust to changes in urinary function and learn how to manage a urinary diversion
- Patient may experience emotional and psychological challenges related to body image, self-esteem, and intimacy
- Patient may undergo follow-up appointments and surveillance to monitor for recurrence or complications
- Patient may need ongoing support from healthcare providers, support groups, or mental health professionals to cope with the physical and emotional effects of surgery.
What to Ask Your Doctor
- What are the potential risks and complications associated with a cystectomy procedure?
- How will my urinary function be affected after a cystectomy?
- What are the options for urinary diversion after a cystectomy, such as an ileal conduit or neobladder, and what are the differences between them?
- How will my sexual function be impacted by a cystectomy?
- What support services are available to help me cope with the emotional and psychological effects of a cystectomy?
- How long is the recovery process after a cystectomy, and what can I expect during this time?
- Are there any alternative treatment options to consider besides a cystectomy?
- How often will I need follow-up appointments or monitoring after a cystectomy?
- How will a cystectomy affect my overall quality of life, and what can I do to maintain or improve it post-surgery?
- Are there any lifestyle changes or precautions I should take after a cystectomy to optimize my health and well-being?
Reference
Authors: Tyson MD 2nd, Barocas DA. Journal: Urol Clin North Am. 2018 May;45(2):249-256. doi: 10.1016/j.ucl.2017.12.008. Epub 2018 Feb 21. PMID: 29650140