Our Summary
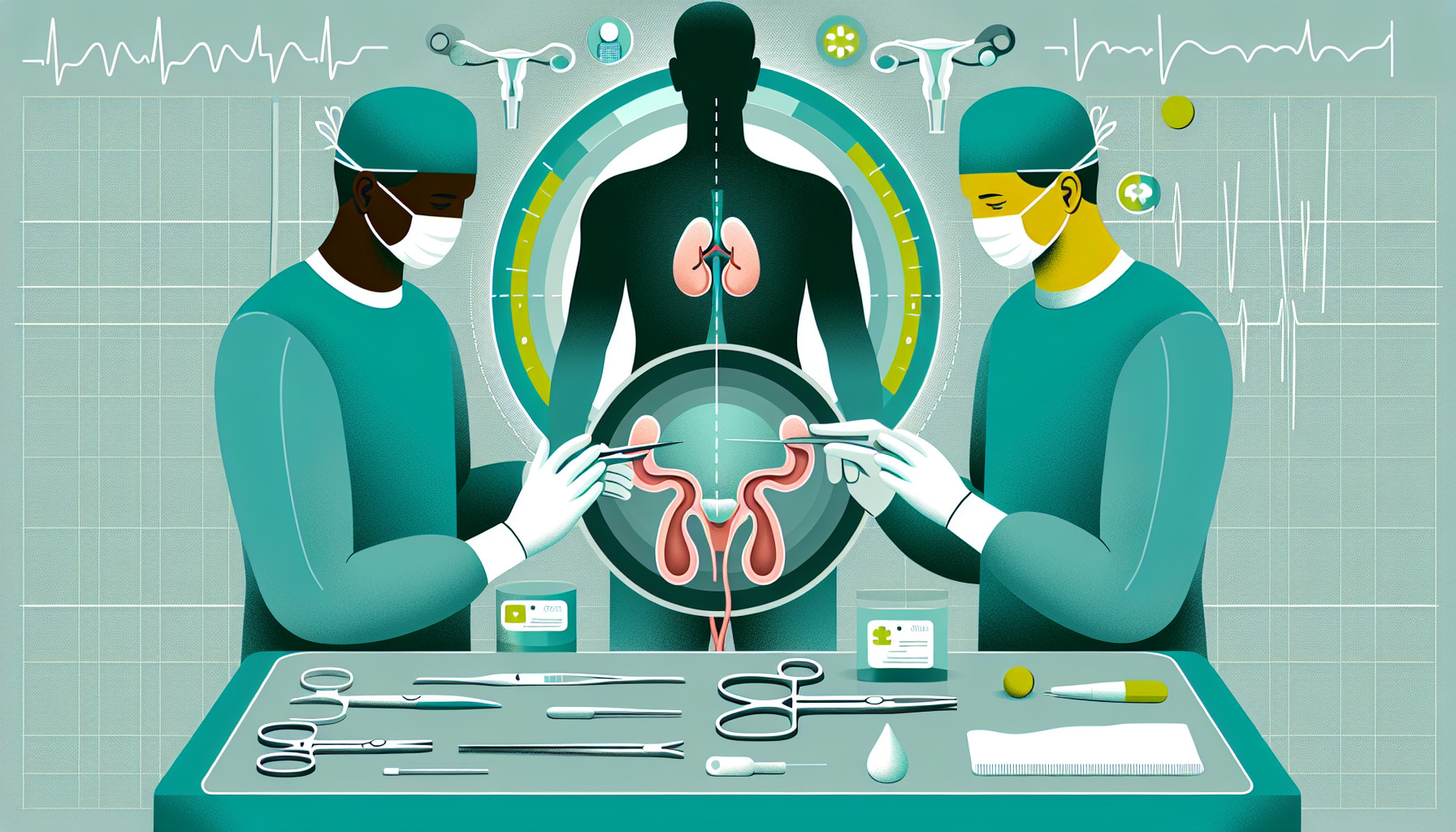
This research paper talks about parastomal hernia, a common problem that often occurs after a specific type of urinary surgery where a small opening (stoma) is created in the abdomen. This hernia can cause various issues such as pain, leakage, and in rare cases, bowel obstruction. It is reported that the rates of this hernia can be as high as 65% and in some cases, about 30% of patients might need another surgery to fix it. Traditional methods to fix this problem have not been very successful, with the problem recurring in 30-76% of cases.
Given the high rates of recurrence and associated health risks, doctors are now trying to prevent it during the initial surgery itself. One such method involves placing a mesh around the stoma at the time of the surgery. Studies have shown that this method significantly reduces the chances of getting a hernia later on. The paper reports that this method was found to be safe and effective in reducing the hernia rates, at least in the short-term. The paper reviews this condition, the risk factors associated with it, and discusses the use of this mesh during the surgery to prevent this problem.
FAQs
- What is a parastomal hernia and what problems can it cause?
- What is the traditional method of fixing a parastomal hernia and how successful has it been?
- What new method are doctors using to prevent parastomal hernias during the initial surgery and how effective is it?
Doctor’s Tip
When discussing cystectomy with a patient, a doctor might advise them about the risk of developing a parastomal hernia and the potential benefits of using a mesh during the surgery to prevent it. This proactive approach can help reduce the likelihood of experiencing complications and the need for additional surgeries in the future. It is important for patients to discuss this option with their healthcare provider and weigh the potential benefits against any potential risks associated with the use of a mesh.
Suitable For
Patients who have undergone urinary surgery that involves creating a stoma in the abdomen are typically recommended cystectomy. This includes patients who have had a urostomy, ileal conduit, or other urinary diversion surgeries. These patients are at a higher risk of developing a parastomal hernia, and cystectomy with mesh placement can help prevent this complication. Additionally, patients who have already developed a parastomal hernia may also be recommended cystectomy to repair the hernia and prevent further complications.
Timeline
Before cystectomy:
- Patient is diagnosed with bladder cancer or other conditions that require cystectomy.
- Patient undergoes pre-operative evaluations and tests to assess their overall health and readiness for surgery.
- Patient meets with their healthcare team to discuss the procedure, risks, benefits, and potential complications.
- Patient undergoes cystectomy surgery to remove the bladder and possibly nearby organs or tissues.
- Patient may receive a urinary diversion procedure to create a new way for urine to leave the body (such as an ileal conduit or continent urinary diversion).
After cystectomy:
- Patient may experience pain, discomfort, and fatigue post-surgery.
- Patient recovers in the hospital for a period of time before being discharged.
- Patient may need to adjust to changes in urinary function and learn how to manage their urinary diversion.
- Patient may experience complications such as infection, blood clots, or parastomal hernia in the months or years following surgery.
- If a parastomal hernia occurs, patient may require additional surgery or treatment to repair the hernia and alleviate symptoms.
Overall, the patient’s experience before and after cystectomy involves a series of medical evaluations, surgical procedures, recovery, and potential complications that require ongoing monitoring and management by healthcare providers.
What to Ask Your Doctor
Some questions a patient should ask their doctor about cystectomy and the potential risk of developing a parastomal hernia include:
- What is a parastomal hernia and what are the symptoms I should watch out for?
- What are the risk factors for developing a parastomal hernia after a cystectomy?
- What is the likelihood of me developing a parastomal hernia after my surgery?
- What are the potential complications of a parastomal hernia?
- What are the traditional methods used to treat a parastomal hernia?
- What is the success rate of using a mesh to prevent a parastomal hernia during the initial surgery?
- Are there any potential risks or complications associated with using a mesh during the surgery?
- How long does the mesh need to stay in place and what is the follow-up care required?
- What can I do to reduce my risk of developing a parastomal hernia after surgery?
- How often will I need to be monitored for the development of a parastomal hernia post-surgery?
Reference
Authors: Donahue TF, Bochner BH. Journal: Investig Clin Urol. 2016 Jul;57(4):240-8. doi: 10.4111/icu.2016.57.4.240. Epub 2016 Jul 5. PMID: 27437533