Our Summary
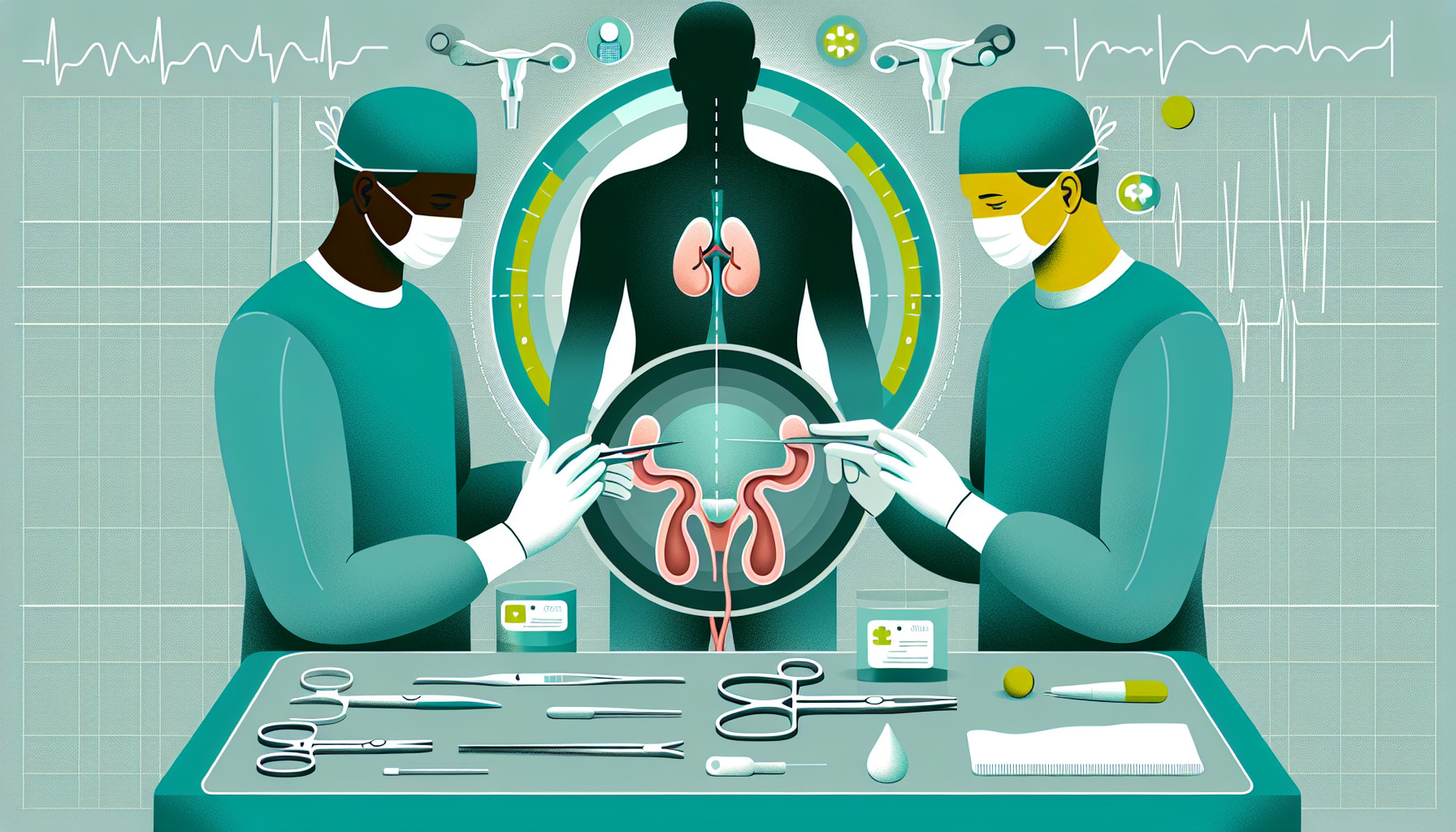
This research paper compares two methods of treating bladder cancer: robotic-assisted radical cystectomy (RARC) and laparoscopic radical cystectomy (LRC). The researchers looked at factors such as operation time, blood loss during surgery, the time it took for patients to start eating again after surgery, how long they stayed in the hospital, and complications that arose.
They found that there wasn’t a significant difference in effectiveness or safety between the two methods. This suggests that for hospitals that don’t have the capability to perform robot-assisted surgeries, LRC may be a good alternative for a less invasive surgery with a quicker recovery time. However, the researchers emphasize that their conclusions need to be backed up by more studies with a larger number of patients, a more rigorous design, and longer follow-up periods.
FAQs
- What were the two methods of treating bladder cancer compared in the research?
- Did the research find a significant difference in effectiveness or safety between robotic-assisted radical cystectomy (RARC) and laparoscopic radical cystectomy (LRC)?
- What were the factors considered by the researchers in comparing the two methods of bladder cancer treatment?
Doctor’s Tip
One helpful tip a doctor might tell a patient about cystectomy is to follow post-operative care instructions carefully to ensure a smooth recovery. This may include taking prescribed medications, avoiding strenuous activities, and attending follow-up appointments with your healthcare provider. It is also important to communicate any concerns or changes in symptoms to your doctor promptly.
Suitable For
Patients with bladder cancer who are recommended for cystectomy typically have high-grade, invasive tumors that have not responded to other treatments such as chemotherapy or radiation therapy. Additionally, patients with recurrent bladder cancer or those with non-muscle invasive bladder cancer that has progressed to muscle invasion may also be recommended for cystectomy. Other factors that may influence the recommendation for cystectomy include the patient’s overall health and ability to undergo surgery, as well as their preferences and goals for treatment.
Timeline
- Before cystectomy:
- Patient is diagnosed with bladder cancer and undergoes various tests and evaluations to determine the stage and extent of the cancer.
- Patient may undergo chemotherapy or radiation therapy to shrink the tumor before surgery.
- Patient meets with a surgeon to discuss the procedure, potential risks and benefits, and post-operative care.
- Patient undergoes pre-operative preparations such as fasting, bowel prep, and medication adjustments.
- Patient undergoes the cystectomy procedure.
- After cystectomy:
- Patient wakes up in the recovery room and is closely monitored for any complications.
- Patient may experience pain, discomfort, and fatigue in the days following surgery.
- Patient is gradually introduced to a liquid diet and then solid foods as tolerated.
- Patient may need to use a urinary diversion system such as a urostomy bag.
- Patient undergoes physical therapy and rehabilitation to regain strength and function.
- Patient is discharged from the hospital and continues to follow up with their healthcare team for monitoring and follow-up care.
- Patient may experience changes in body image, emotional challenges, and adjustment to a new way of life post-cystectomy.
What to Ask Your Doctor
- What is the success rate of cystectomy in treating bladder cancer?
- What are the potential risks and complications associated with cystectomy?
- How long is the recovery period after cystectomy?
- Will I need any additional treatments or follow-up care after the surgery?
- Are there any alternative treatments to consider before opting for cystectomy?
- What is the difference between robotic-assisted cystectomy and laparoscopic cystectomy in terms of outcomes and recovery?
- How experienced is the surgical team in performing cystectomy procedures?
- What is the expected outcome in terms of quality of life after cystectomy?
- How will my bladder function be affected after cystectomy, and what are the options for bladder reconstruction or urinary diversion?
- Are there any clinical trials or new technologies available for cystectomy that I should consider?
Reference
Authors: Peng L, Li J, Cao D, Ren Z, Wei T, You C, Cheng B, Wei Q, Li Y. Journal: J Cancer Res Clin Oncol. 2020 Jun;146(6):1591-1601. doi: 10.1007/s00432-020-03183-0. Epub 2020 Mar 17. PMID: 32185487