Our Summary
This research paper is a thorough review of other studies done on how certain types of jaw surgery might affect the process of root resorption, which is when the body naturally gets rid of tooth root tissue. The authors sifted through various databases for related articles until April 2022 and ended up using six different articles for their review.
Most of the studies they reviewed were looking back at past data, but one was a clinical trial. They followed up with the patients for anywhere between six months to ten years after their surgeries. The majority of the studies used 2D imaging to measure root resorption, but one used a more advanced 3D imaging technique known as cone-beam computed tomography (CBCT).
The results showed that about 1 to 36% of teeth were affected by root resorption after the surgeries, with certain procedures like surgically assisted rapid maxillary expansion (SARME) and Le Fort I osteotomy causing the most resorption.
However, the authors note that more research is needed, particularly studies that use CBCT, to get a better understanding of how different types of jaw surgery can lead to root resorption.
FAQs
- What is the main focus of the research paper on orthognathic surgery?
- What were the primary findings regarding root resorption after jaw surgery?
- Why do the authors of the study suggest the need for more research using CBCT?
Doctor’s Tip
One helpful tip a doctor might give to a patient considering orthognathic surgery is to make sure to follow post-operative care instructions carefully. This may include maintaining good oral hygiene, avoiding hard or crunchy foods, attending follow-up appointments, and taking any prescribed medications as directed. Following these instructions can help ensure a successful recovery and minimize the risk of complications such as root resorption.
Suitable For
Overall, orthognathic surgery is typically recommended for patients with severe jaw discrepancies, such as:
Facial asymmetry: Patients with significant differences in the size or positioning of their jaws may benefit from orthognathic surgery to correct the imbalance and improve facial aesthetics.
Malocclusion: Patients with severe misalignment of the teeth and jaws, such as overbite, underbite, or crossbite, may require orthognathic surgery to realign the jaws and improve bite function.
Sleep apnea: Some patients with obstructive sleep apnea may benefit from orthognathic surgery to reposition the jaws and improve airway function, reducing the symptoms of sleep apnea.
Temporomandibular joint (TMJ) disorders: Patients with TMJ disorders that are caused by jaw misalignment or dysfunction may benefit from orthognathic surgery to correct the underlying issue and alleviate symptoms.
Facial trauma: Patients who have sustained facial trauma resulting in severe damage to the jaws may require orthognathic surgery to reconstruct and restore function to the affected areas.
It is important for patients considering orthognathic surgery to undergo a comprehensive evaluation by a team of oral and maxillofacial surgeons, orthodontists, and other specialists to determine if surgery is the best treatment option for their specific condition.
Timeline
Before orthognathic surgery, a patient will typically undergo a series of consultations with an orthodontist and oral and maxillofacial surgeon to determine the need for surgery and create a treatment plan. This may include orthodontic treatment to align the teeth properly before surgery. The patient will also undergo various imaging tests such as X-rays and CT scans to assess the jaw structure.
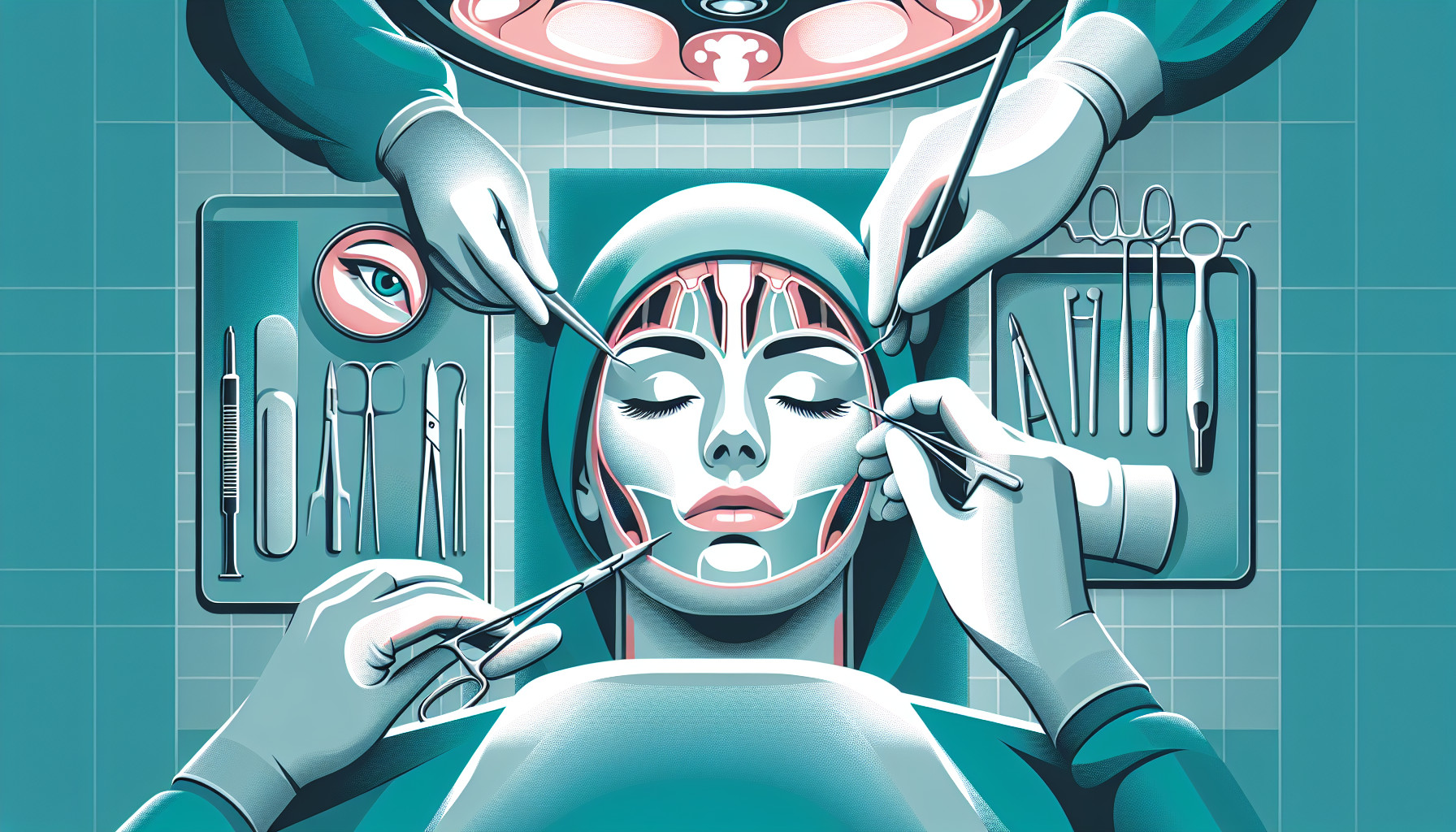
On the day of surgery, the patient will be placed under general anesthesia, and the surgeon will make incisions in the jaw to reposition the bones. The surgery can take several hours, and the patient will need to stay in the hospital for a few days for monitoring.
After surgery, the patient will experience swelling, pain, and bruising, which can last for several weeks. They will need to follow a strict diet of soft foods and avoid strenuous activities. Follow-up appointments will be scheduled to monitor the healing process and make any necessary adjustments to the treatment plan.
Over the next several months, the patient will continue to see their orthodontist for adjustments to their braces or aligners to ensure proper alignment of the teeth. It can take up to a year or more for the full results of the surgery to be visible.
Overall, the timeline for a patient before and after orthognathic surgery can vary depending on the individual case, but the process typically involves thorough planning, surgery, and post-operative care to achieve the desired results.
What to Ask Your Doctor
- What specific type of orthognathic surgery do you recommend for my condition?
- What are the potential risks and complications associated with orthognathic surgery, including the risk of root resorption?
- How will orthognathic surgery affect my bite and jaw function?
- What is the expected recovery time and post-operative care for orthognathic surgery?
- Will I need braces or other orthodontic treatment before or after the surgery?
- How long will the effects of orthognathic surgery last?
- Are there any alternative treatments or procedures that could achieve similar results?
- How many times have you performed this type of surgery, and what is your success rate?
- What can I do to prepare for orthognathic surgery, both physically and mentally?
- Are there any long-term implications or considerations I should be aware of before undergoing orthognathic surgery?
Reference
Authors: Alqahtani KA, Shaheen E, Morgan N, Shujaat S, Politis C, Jacobs R. Journal: J Stomatol Oral Maxillofac Surg. 2022 Oct;123(5):e260-e267. doi: 10.1016/j.jormas.2022.04.010. Epub 2022 Apr 25. PMID: 35477011