Our Summary
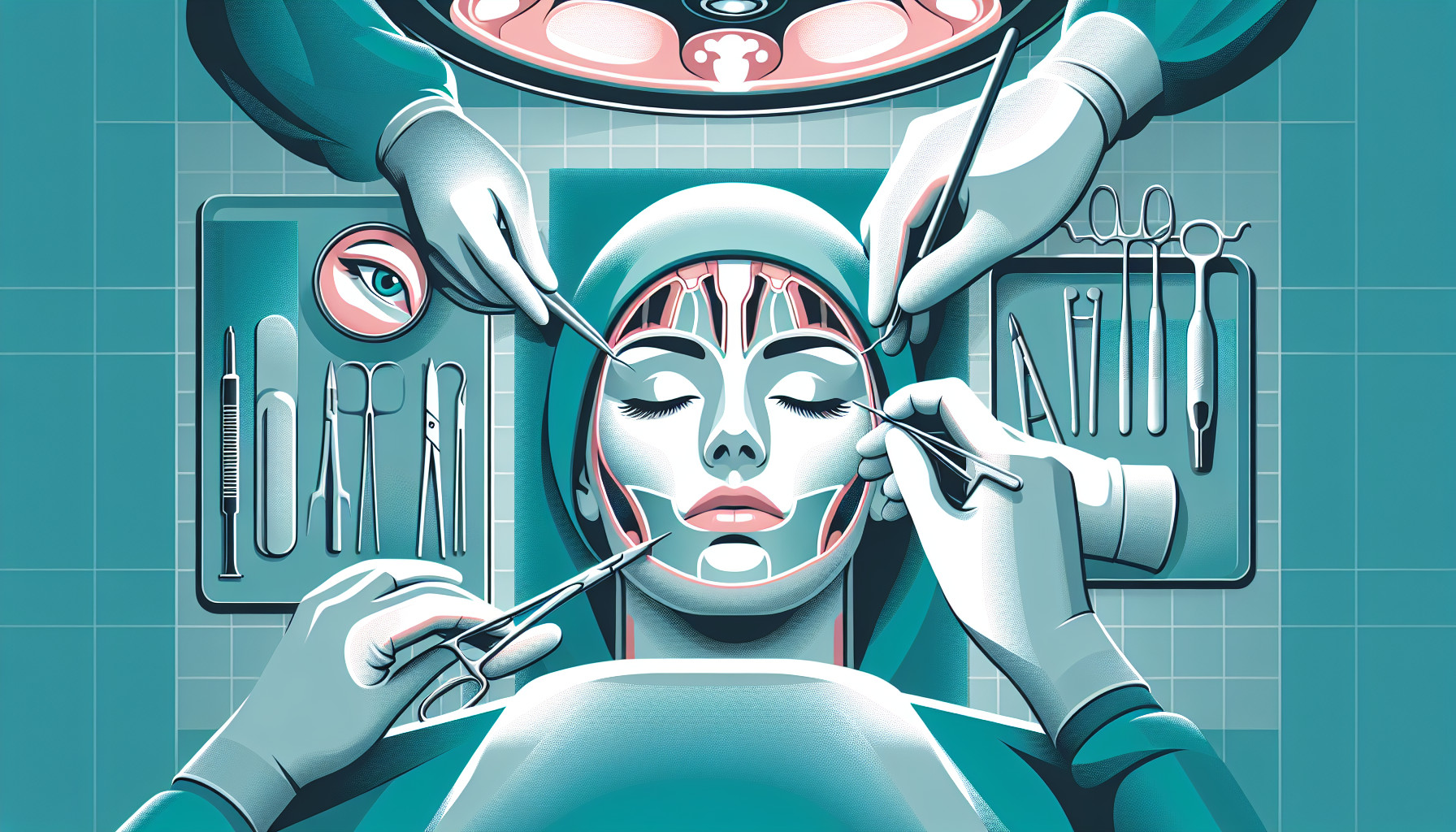
This research paper reviews the negative side effects and complications that can occur from orthognathic surgery, which is surgery to correct conditions of the jaw and face related to structure, growth, sleep apnea, TMJ disorders, malocclusion problems owing to skeletal disharmonies, or other orthodontic problems that cannot be easily treated with braces. The study looked back at 10 years of patient data, from 2009 to 2018.
Several factors, such as the patient’s sex, age, pre-surgery conditions, diagnosis, type of surgery, amount of bleeding, length of surgery, and length of hospitalization, were considered in this study. A total of 891 patients (39.1% male, 60.9% female) with an average age of 26.4 years were included.
The most common immediate side effect after surgery was a disturbance of the senses, such as touch or taste, in 93.5% of patients. The four most common complications were a relapse (6.4%), post-operative temporomandibular joint disorder (TMD, a type of jaw pain, 5.7%), unfavorable bone cutting (5.5%), and infection (4.9%). These complications were more common in males.
On average, patients lost about 497 ml of blood during surgery and the operations lasted about 401 minutes. The amount of blood loss, length of surgery, and type of skeletal deformity significantly affected the rate of complications. No fatal complications were reported.
The study concludes that the length of the operation is a significant factor in complications. However, several other factors could be adjusted to reduce the rate of complications and improve treatment outcomes.
FAQs
- What are the most common complications of orthognathic surgery?
- Does the duration of the operation influence the rate of complications in orthognathic surgery?
- How does the type of skeletal deformity affect the complication rates in orthognathic surgery?
Doctor’s Tip
A helpful tip a doctor might tell a patient about orthognathic surgery is to follow all pre-operative and post-operative instructions closely to help prevent complications and ensure a successful outcome. This may include maintaining good oral hygiene, avoiding certain foods or activities, taking prescribed medications as directed, attending follow-up appointments, and following a proper diet plan. It is also important to communicate openly with your healthcare team about any concerns or questions you may have during the recovery process.
Suitable For
Orthognathic surgery is typically recommended for patients with dentofacial deformities, such as skeletal discrepancies, malocclusions, and facial asymmetry. Patients with severe overbites, underbites, crossbites, open bites, and other jaw misalignments may benefit from orthognathic surgery to improve their bite, facial aesthetics, and overall oral health. Additionally, patients with temporomandibular joint disorders (TMD) or obstructive sleep apnea may also be candidates for orthognathic surgery to correct underlying structural issues contributing to their condition. It is important for patients considering orthognathic surgery to undergo a thorough evaluation by a maxillofacial surgeon to determine if they are suitable candidates for the procedure.
Timeline
Before orthognathic surgery:
- Patient undergoes a comprehensive evaluation by an orthodontist and oral and maxillofacial surgeon
- Pre-operative orthodontic treatment to align teeth and prepare for surgery
- Pre-surgical orthodontic records including X-rays, photographs, and dental impressions are taken
- Surgical planning and discussion of treatment goals with the patient
- Pre-operative medical clearance and lab work
- Discussion of potential risks and complications of surgery
After orthognathic surgery:
- Patient undergoes the surgical procedure under general anesthesia
- Post-operative pain management and monitoring in the hospital
- Initial swelling and discomfort in the first few days after surgery
- Follow-up appointments with the surgeon and orthodontist for post-operative care and adjustments
- Gradual improvement in facial appearance and function over several weeks to months
- Long-term follow-up for monitoring of results and potential complications
- Orthodontic treatment continues to finalize the bite and alignment of teeth
Overall, orthognathic surgery is a complex and multi-step process that requires careful planning, collaboration between multiple healthcare providers, and dedication from the patient to achieve optimal results.
What to Ask Your Doctor
- What are the potential risks and complications associated with orthognathic surgery?
- How experienced are you in performing orthognathic surgery procedures?
- What type of anesthesia will be used during the surgery?
- How long will the surgery take and what is the expected recovery time?
- What post-operative care will be required and what can I expect during the recovery process?
- Will I experience any changes in sensation or function in my face and jaw after surgery?
- What are the chances of relapse or the need for additional procedures in the future?
- How will my bite and facial appearance be affected by the surgery?
- Are there any alternative treatment options available for my condition?
- Can you provide me with information about your success rates and patient outcomes with orthognathic surgery?
Reference
Authors: Damrongsirirat N, Kaboosaya B, Siriwatana K, Subbalekha K, Jansisyanont P, Pimkhaokham A. Journal: J Craniomaxillofac Surg. 2022 Mar;50(3):197-203. doi: 10.1016/j.jcms.2021.11.011. Epub 2021 Dec 2. PMID: 34876326