Our Summary
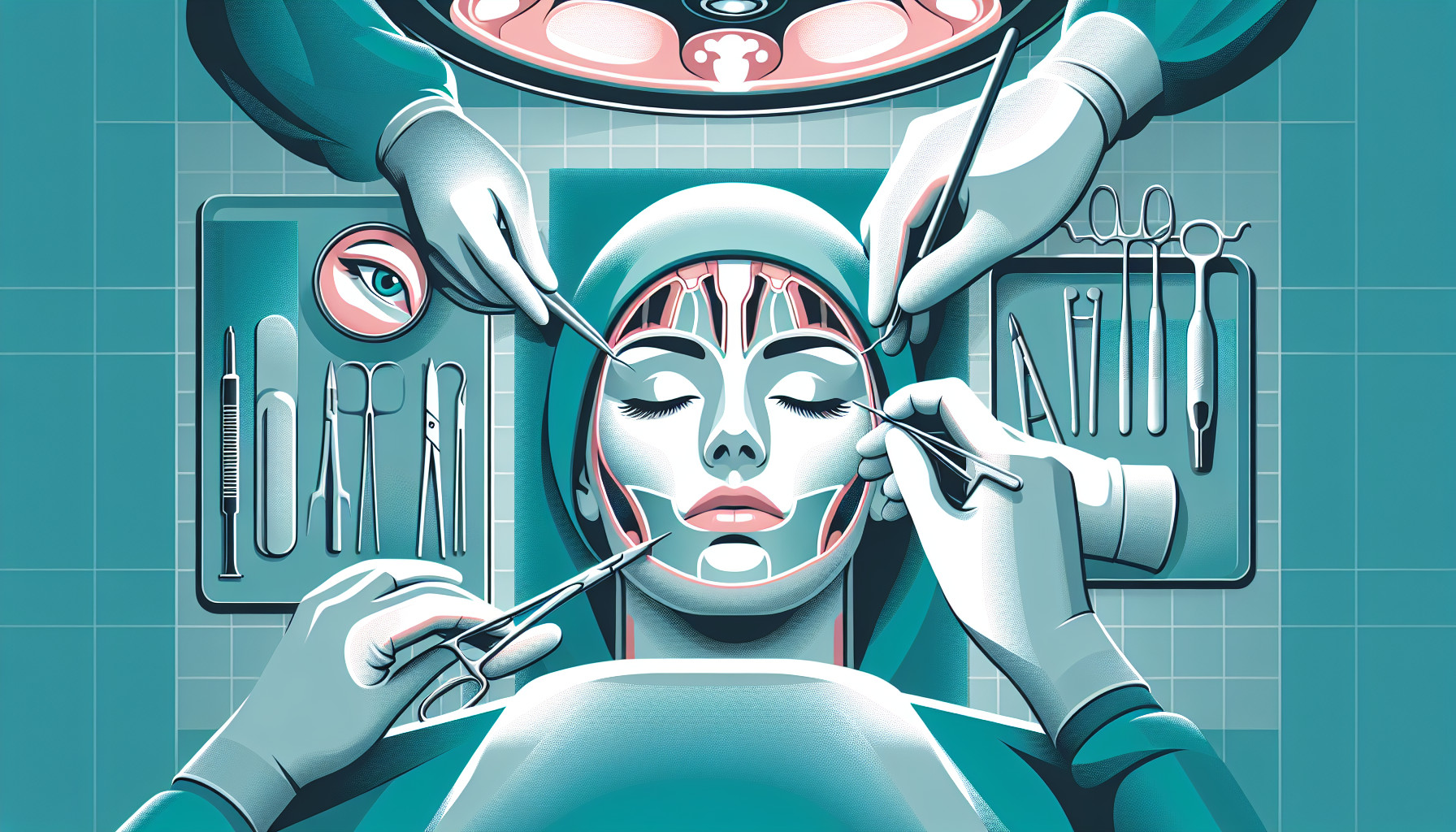
This research paper looks at the impact of virtual surgical planning (VSP) on orthognathic surgery, which is surgery to correct conditions of the jaw and face related to structure, growth, sleep apnea, TMJ disorders, malocclusion problems owing to skeletal disharmonies, or other orthodontic problems that cannot be easily treated with braces.
The researchers examined how surgeons trained in plastic and reconstructive surgery (PRS) or oral and maxillofacial surgery (OMS) have been using VSP and how it has influenced their research and practices.
They found that the use of VSP has been growing since its first introduction in 2000, but the rate of adoption and focus of research varies between the two groups of surgeons. For instance, PRS surgeons have been slower in publishing research on VSP and have focused more on its aesthetic applications compared to OMS surgeons.
Moreover, they found that a significant majority (over 80.6%) of all orthognathic surgery literature was published after 2008, which is when VSP was first integrated into orthognathic surgery.
The study concludes that VSP has had a varied impact on orthognathic surgery research depending on the surgeon’s training. However, more research is needed to understand how VSP has affected actual clinical practices in PRS and OMS.
FAQs
- What is virtual surgical planning (VSP) and how is it used in orthognathic surgery?
- How has the use and research of VSP varied between plastic and reconstructive surgery (PRS) and oral and maxillofacial surgery (OMS)?
- When was VSP first integrated into orthognathic surgery and what impact has it had on the field?
Doctor’s Tip
One helpful tip a doctor might tell a patient about orthognathic surgery is to follow post-operative instructions carefully to ensure proper healing and successful results. This may include following a specific diet, avoiding certain activities, and attending follow-up appointments as scheduled. It is important to communicate any concerns or questions with your healthcare provider throughout the recovery process.
Suitable For
Patients who are typically recommended orthognathic surgery include those with:
Severe malocclusion: Orthognathic surgery may be recommended for patients with severe misalignment of the teeth and jaws that cannot be corrected with orthodontic treatment alone.
Facial asymmetry: Patients with significant facial asymmetry due to a misalignment of the jaws may benefit from orthognathic surgery to improve their facial appearance and function.
Sleep apnea: Orthognathic surgery can be used to treat obstructive sleep apnea by repositioning the jaw to open up the airway and improve breathing during sleep.
Temporomandibular joint (TMJ) disorders: Patients with TMJ disorders that are caused by a misalignment of the jaws may benefit from orthognathic surgery to correct the underlying structural issue.
Skeletal disharmonies: Patients with skeletal disharmonies, such as a protruding or recessed jaw, may benefit from orthognathic surgery to improve facial aesthetics and function.
Difficulty chewing or swallowing: Patients who have difficulty chewing or swallowing due to a misalignment of the jaws may benefit from orthognathic surgery to improve their ability to eat and speak.
Overall, orthognathic surgery is recommended for patients who have structural or functional issues with their jaws and face that cannot be effectively treated with orthodontic treatment alone.
Timeline
Before orthognathic surgery:
- Patient undergoes initial consultation with orthodontist and oral surgeon to discuss treatment options and create a treatment plan.
- Patient undergoes orthodontic treatment to align teeth and prepare for surgery.
- Patient undergoes pre-surgical orthodontic planning and imaging (such as X-rays, CT scans, and 3D models) to plan the surgery.
- Virtual surgical planning (VSP) is used to simulate the surgery and create a surgical plan.
- Patient undergoes final pre-surgical orthodontic adjustments.
After orthognathic surgery:
- Patient undergoes orthognathic surgery to reposition the jaw and/or facial bones.
- Patient spends time in recovery and healing from surgery.
- Patient may need to undergo post-surgical orthodontic adjustments to fine-tune the bite and alignment of the teeth.
- Patient undergoes follow-up appointments with the orthodontist and oral surgeon to monitor healing and progress.
- Patient continues with orthodontic treatment to maintain the results of the surgery and achieve optimal alignment of the teeth and jaw.
What to Ask Your Doctor
Some questions a patient should ask their doctor about orthognathic surgery include:
- What are the potential risks and complications associated with orthognathic surgery?
- What is the recovery process like and how long will it take to fully recover?
- Will I need to wear braces before or after the surgery?
- How will my bite and facial appearance be affected by the surgery?
- What are the alternative treatment options available for my condition?
- How many orthognathic surgeries have you performed and what is your success rate?
- Can you show me before and after photos of patients who have undergone orthognathic surgery?
- Will I need to see a speech therapist or undergo any additional therapy after the surgery?
- How will my insurance coverage work for orthognathic surgery?
- What can I do to prepare for the surgery and optimize my results?
Reference
Authors: Chen J, Abousy M, Girard A, Duclos O, Patel V, Jenny H, Redett R, Yang R. Journal: J Craniofac Surg. 2022 Jul-Aug 01;33(5):1418-1423. doi: 10.1097/SCS.0000000000008607. Epub 2022 Mar 8. PMID: 35258010