Our Summary
This research paper compares two methods of orthognathic surgery, a procedure used to correct facial deformities. The two methods are the traditional one using regular plates and a newer technique using patient-specific osteosynthesis plates (PSOPs). The study looked at whether there were any differences in complications, cost, professional opinions, and patient-reported outcomes between the two methods.
The researchers looked at various sources of information, including published studies, grey literature (like reports and theses), and other databases. They only included randomized and controlled clinical trials in their review.
The results of the study showed that there was no significant difference in the number of complications during and after surgery between the two methods. There was also no significant difference in professional and patient-reported outcomes. However, surgeries using PSOPs did tend to have slightly more reoperations and were significantly more expensive. On the other hand, PSOPs shortened the time for treatment planning and during surgery by about one third compared to the conventional method.
In conclusion, the study did not find significant differences in complications, professional and patient-reported outcomes between the two methods. However, the PSOP method was more expensive but quicker. The researchers suggest that more trials are needed before they can conclusively say which method is better overall.
FAQs
- What are the two methods of orthognathic surgery compared in this study?
- Was there a significant difference in complications and outcomes between the traditional method and the PSOP method?
- How did the cost and duration of the two methods of orthognathic surgery compare in this study?
Doctor’s Tip
One helpful tip a doctor might tell a patient about orthognathic surgery is to carefully weigh the pros and cons of using patient-specific osteosynthesis plates (PSOPs) versus traditional plates. While PSOPs may offer faster treatment planning and surgery time, they may also come with a higher cost and slightly increased risk of reoperations. It’s important for patients to discuss these factors with their surgeon and make an informed decision based on their individual needs and priorities.
Suitable For
Patients who are typically recommended orthognathic surgery are those with facial deformities such as:
- Malocclusion (misalignment of the teeth)
- Jaw discrepancies (overbite, underbite, crossbite)
- Skeletal abnormalities in the face and jaw
- Breathing problems due to facial structure
- Temporomandibular joint disorders
Orthognathic surgery can help improve the function of the jaw, bite, and facial aesthetics in these patients. It is usually recommended after other non-surgical treatments have been attempted and deemed ineffective. The decision to undergo orthognathic surgery is made in collaboration with an orthodontist, oral and maxillofacial surgeon, and other healthcare professionals to ensure the best outcome for the patient.
Timeline
Before orthognathic surgery, a patient typically undergoes a series of consultations with an orthodontist and oral and maxillofacial surgeon to discuss treatment options and create a treatment plan. This may include orthodontic treatment to align the teeth prior to surgery. The patient will also undergo various pre-operative tests and evaluations to ensure they are healthy enough for surgery.
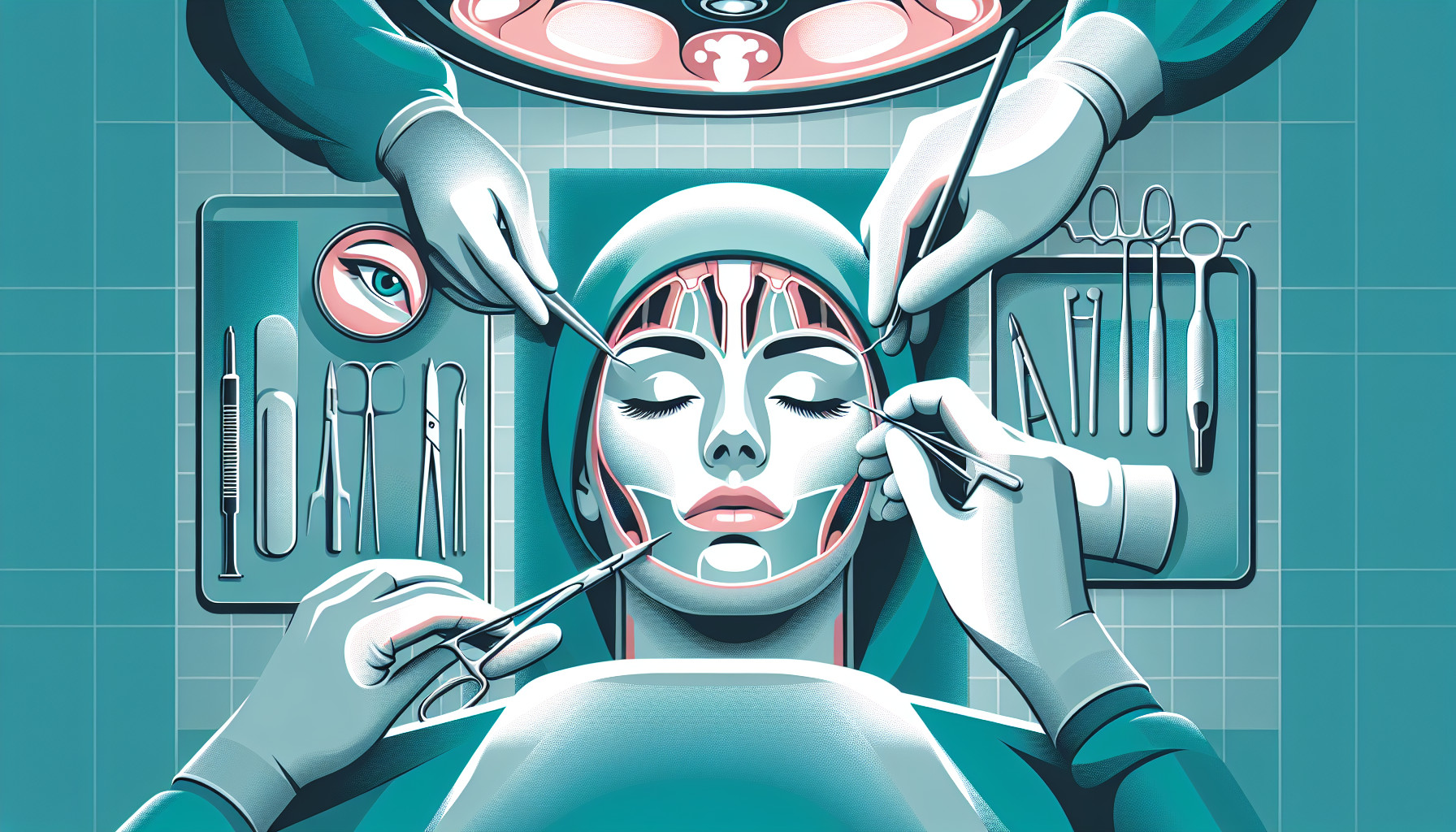
During orthognathic surgery, the surgeon will make incisions in the mouth to access the jawbones. They will then reposition the jawbones to correct the facial deformity. The surgeon may use regular plates or PSOPs to stabilize the bones in their new position. The surgery can take several hours to complete, and the patient will be under general anesthesia.
After orthognathic surgery, the patient will have a recovery period where they may experience swelling, pain, and difficulty eating and speaking. They will need to follow a specific diet and oral hygiene routine to aid in the healing process. The patient will also have follow-up appointments with their surgical team to monitor their progress and make any necessary adjustments to their treatment plan.
Overall, orthognathic surgery is a complex and involved process that requires careful planning and coordination between the patient, orthodontist, and surgeon. With proper care and follow-up, patients can achieve significant improvements in their facial appearance and function.
What to Ask Your Doctor
Some questions a patient should ask their doctor about orthognathic surgery include:
- What are the potential risks and complications associated with orthognathic surgery, and how do they compare between the traditional method using regular plates and the newer method using patient-specific osteosynthesis plates?
- What are the expected outcomes and recovery time for each method of orthognathic surgery?
- Are there any specific criteria that would make me a better candidate for one method over the other?
- How does the cost of surgery differ between the two methods, and what factors should I consider when making a decision based on cost?
- Are there any long-term considerations or differences in the stability of results between the traditional and PSOP methods?
- What is the experience and expertise of the surgical team in performing orthognathic surgery with each method?
- How will the use of PSOPs impact the treatment planning process and overall duration of surgery compared to the traditional method?
- Are there any other alternative treatment options that should be considered before deciding on orthognathic surgery?
- What are the potential benefits and drawbacks of each method in terms of aesthetics and functional outcomes?
- Can I speak with other patients who have undergone orthognathic surgery using each method to hear about their experiences and results?
Reference
Authors: Kesmez Ö, Valls-Ontañón A, Starch-Jensen T, Haas-Junior OL, Hernández-Alfaro F. Journal: Med Oral Patol Oral Cir Bucal. 2022 Nov 1;27(6):e507-e517. doi: 10.4317/medoral.25424. PMID: 36173724