Our Summary
This paper reviews the recent advances in using digital methods to plan how teeth should fit together (known as “occlusion”) in jaw surgery. Currently, there are three methods: manual, semi-automatic, and fully automatic. The manual method relies on visual cues and can be flexible but it’s hard to guarantee the best fit. The semi-automatic method uses computer software for some of the setup, but still relies heavily on manual operation. The fully automatic method uses computer software for the entire process and requires specific programming for different situations.
Initial results show that these digital setup methods are accurate and reliable, but there are still some limitations. More research is needed to understand how these methods affect patient outcomes after surgery, whether doctors and patients accept these methods, and whether they save time and are cost-effective.
FAQs
- What are the three digital methods for planning occlusion in jaw surgery?
- What are the advantages and disadvantages of the manual, semi-automatic, and fully automatic methods for planning occlusion in orthognathic surgery?
- What further research is needed on the use of digital methods in orthognathic surgery?
Doctor’s Tip
A helpful tip a doctor might tell a patient about orthognathic surgery is to follow all pre-operative and post-operative instructions carefully. This may include maintaining good oral hygiene, eating soft foods during the initial recovery period, attending follow-up appointments, and avoiding strenuous activities that could impact the healing process. By following these instructions, patients can help ensure the best possible outcome from their surgery.
Suitable For
Orthognathic surgery is typically recommended for patients with severe jaw misalignment or malocclusion that cannot be corrected with orthodontic treatment alone. This includes patients with:
- Severe overbite or underbite
- Difficulty chewing or speaking due to jaw misalignment
- Facial asymmetry
- Sleep apnea related to jaw position
- Temporomandibular joint (TMJ) disorders
- Difficulty breathing due to a small airway
- Congenital facial deformities
Orthognathic surgery can help improve the function and appearance of the jaw, teeth, and facial structures, leading to better overall oral health and quality of life for these patients.
Timeline
Before orthognathic surgery, a patient typically undergoes a series of consultations with an oral and maxillofacial surgeon, orthodontist, and other specialists to determine the need for surgery and develop a treatment plan. This may include orthodontic treatment to align the teeth properly before surgery.
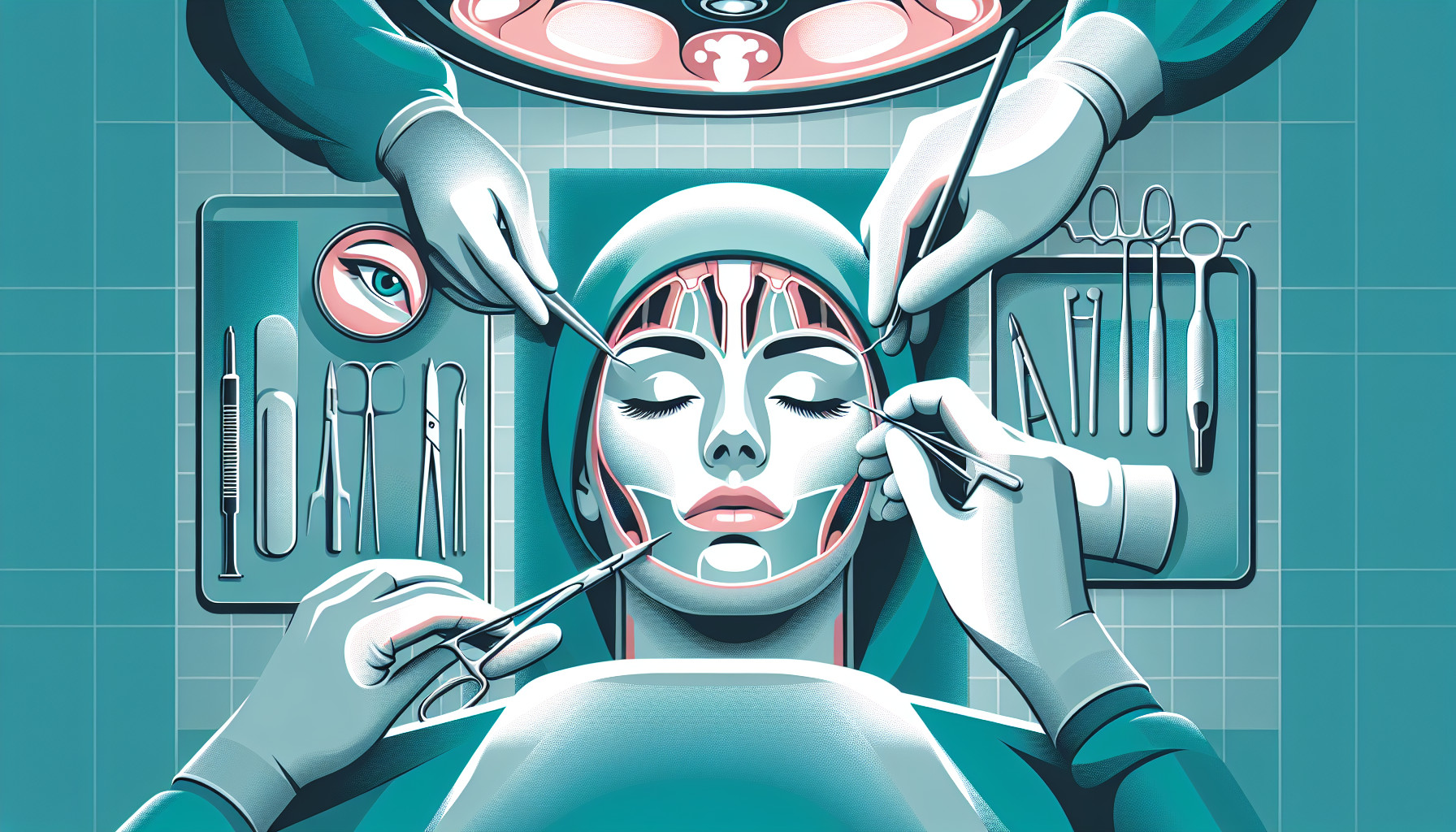
During the surgery, the surgeon will make incisions in the jawbone to reposition the upper and lower jaws as needed. This may involve cutting and reshaping the bone to achieve the desired alignment. The surgery is usually performed under general anesthesia and can take several hours to complete.
After surgery, the patient will experience swelling, bruising, and discomfort in the jaw and facial area. Pain medication and a soft diet may be prescribed to help manage these symptoms. The patient will also need to follow a strict post-operative care plan, which may include wearing elastics or braces to help stabilize the jaws in their new position.
Over the following weeks and months, the patient will attend follow-up appointments with their surgical team to monitor healing and make any necessary adjustments to the treatment plan. Orthodontic treatment may continue after surgery to further refine the alignment of the teeth.
Ultimately, the goal of orthognathic surgery is to improve the patient’s bite, facial aesthetics, and overall oral health. With proper planning and post-operative care, patients can achieve long-lasting results and a more functional and harmonious smile.
What to Ask Your Doctor
- What are the potential benefits of orthognathic surgery for my specific case?
- What are the risks and potential complications associated with orthognathic surgery?
- How long is the recovery process and what can I expect in terms of pain and discomfort?
- Will I need any additional procedures or treatments before or after the surgery?
- How will my bite be affected by the surgery and what can I expect in terms of changes to my jaw alignment?
- What are the success rates for orthognathic surgery and what is the likelihood of needing additional surgeries in the future?
- How will my appearance be affected by the surgery and what are the potential aesthetic outcomes?
- What are the alternatives to orthognathic surgery and how do they compare in terms of effectiveness and risks?
- Can you provide me with information on the digital methods used for planning my surgery and how they may impact the outcome?
- Do you have experience performing orthognathic surgery and what is your success rate with this procedure?
Reference
Authors: Li L, Niu F. Journal: Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2023 Feb 15;37(2):247-251. doi: 10.7507/1002-1892.202210086. PMID: 36796824