Our Summary
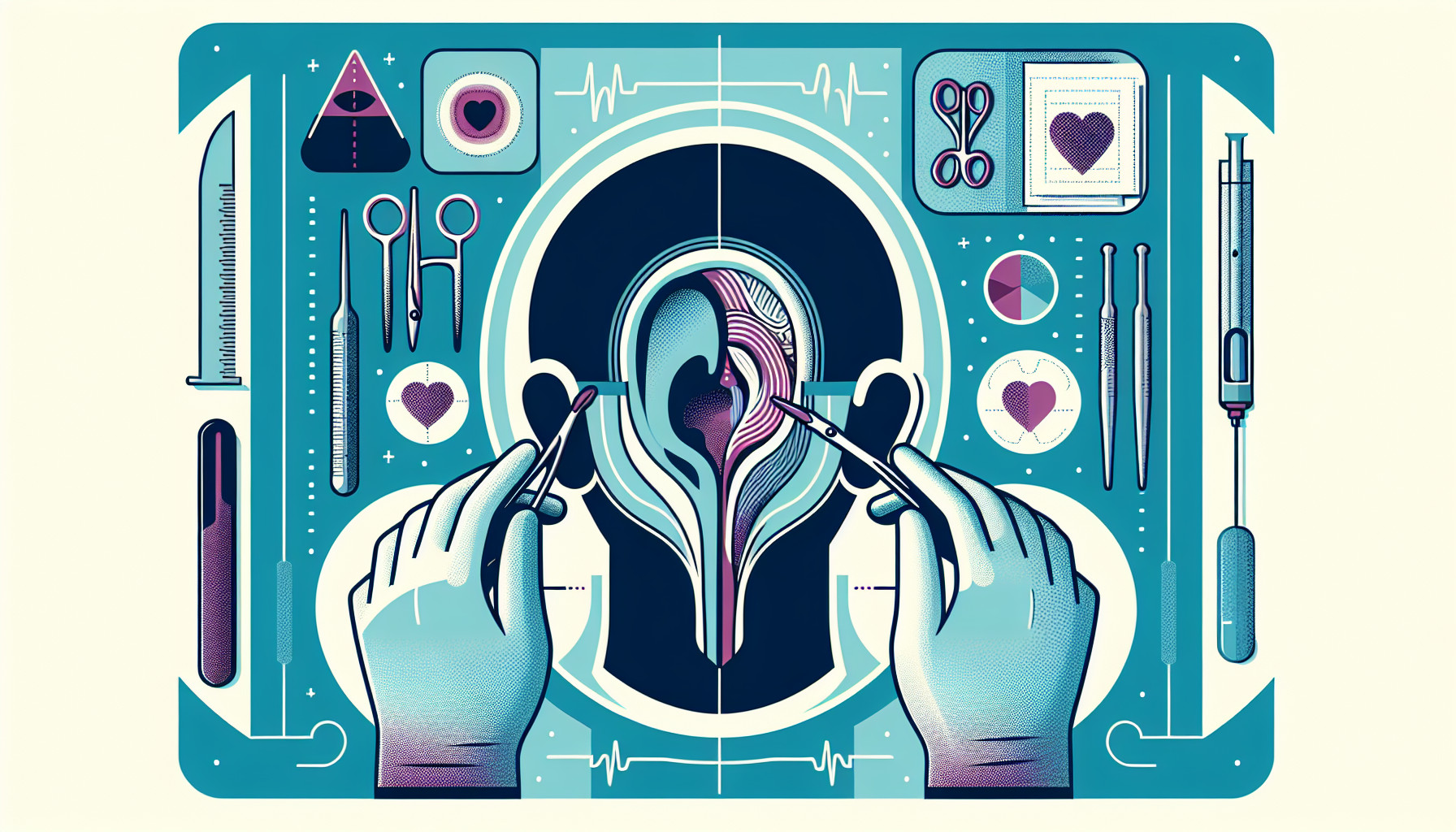
This research paper investigates the connection between ear problems (Eustachian tube dysfunction or ETD) and sinus infections (chronic rhinosinusitis or CRS). The study looks at whether these conditions when they occur together (CRS+ETD) are similar to ETD occurring by itself (primary ETD), and how they respond to different treatments.
The researchers reviewed 16 previous studies involving over 1,500 patients. They found that about half of the patients with sinus infections also had ETD. When comparing the severity of ETD in patients with both conditions to those with ETD alone, they found that those with ETD alone had worse symptoms.
In terms of treatment, patients with both CRS and ETD who underwent sinus surgery alone showed significant improvements, similar to those of patients with ETD alone who were treated with a specific procedure involving balloon dilation of the Eustachian tube.
In simple terms, if you have a sinus infection, there’s a good chance you might also have problems with your ears, but the ear problems are usually more severe if you don’t also have a sinus infection. Both conditions can be effectively treated with their respective procedures.
FAQs
- What is the connection between ear problems (Eustachian tube dysfunction or ETD) and sinus infections (chronic rhinosinusitis or CRS)?
- Are the symptoms of ETD more severe in patients who also have CRS or in those who only have ETD?
- How effective are the treatments for patients suffering from both CRS and ETD compared to those with ETD alone?
Doctor’s Tip
One helpful tip a doctor might give a patient about ear tube surgery is to follow post-operative care instructions carefully. This may include keeping the ears dry, avoiding swimming or getting water in the ears, and attending follow-up appointments as scheduled. It is also important to be aware of any signs of infection or complications, such as persistent pain, drainage from the ear, or hearing loss, and to contact your doctor if you experience any of these symptoms. By following these guidelines, you can help ensure a successful recovery from ear tube surgery.
Suitable For
Patients who are typically recommended ear tube surgery include those with chronic Eustachian tube dysfunction (ETD) that does not improve with other treatments such as nasal decongestants, antihistamines, or nasal steroids. Symptoms of ETD include persistent ear pain, pressure, and fluid buildup in the middle ear, which can lead to hearing loss and recurrent ear infections.
Children are more commonly recommended for ear tube surgery as they are more prone to ETD due to their smaller, more horizontal Eustachian tubes which can become blocked more easily. Children who have had multiple ear infections or persistent fluid in the middle ear may benefit from ear tube surgery to improve their hearing and reduce the risk of future infections.
Adults may also be recommended for ear tube surgery if they have chronic ETD that affects their quality of life, such as frequent ear infections, hearing loss, or dizziness. Other conditions that may warrant ear tube surgery in adults include barotrauma (ear pain or pressure changes during air travel or scuba diving) or Eustachian tube dysfunction related to allergies or sinus infections.
Overall, patients who are recommended for ear tube surgery are those who have persistent or severe symptoms of ETD that impact their daily functioning and quality of life, and who have not responded to other conservative treatments. It is important to consult with an ear, nose, and throat specialist to determine if ear tube surgery is the best option for you based on your individual symptoms and medical history.
Timeline
Before ear tube surgery:
- Patient experiences symptoms such as recurrent ear infections, fluid buildup in the middle ear, hearing loss, and balance issues.
- Patient visits an ear, nose, and throat (ENT) specialist who diagnoses ETD and recommends ear tube surgery as a treatment option.
- Patient undergoes preoperative evaluations, such as hearing tests and a physical examination, to assess their candidacy for ear tube surgery.
After ear tube surgery:
- Patient undergoes a relatively quick and minimally invasive surgical procedure to insert tiny tubes into the eardrums to help drain fluid and equalize pressure in the middle ear.
- Patient may experience some discomfort and ear drainage immediately after the surgery, which typically resolves within a few days.
- Patient follows postoperative care instructions provided by the ENT specialist, which may include avoiding water in the ears, using ear drops, and attending follow-up appointments.
- Patient experiences improvement in their ear symptoms, such as reduced frequency of ear infections, improved hearing, and overall better ear health.
What to Ask Your Doctor
Some questions a patient should ask their doctor about ear tube surgery include:
- What are the benefits of ear tube surgery for my specific condition?
- What are the risks and potential complications of ear tube surgery?
- How long does the procedure take, and what is the recovery process like?
- Will I need to follow any special precautions or restrictions after the surgery?
- How long do ear tubes typically stay in place, and will I need to have them removed in the future?
- Will ear tube surgery improve my hearing or help with other ear-related symptoms?
- Are there any alternative treatments or options I should consider before deciding on ear tube surgery?
- What is the success rate of ear tube surgery for patients with my condition?
- How often will I need to follow up with you after the surgery?
- Are there any specific lifestyle changes or habits I should adopt to help maintain the effectiveness of the ear tubes?
Reference
Authors: Chen T, Shih MC, Edwards TS, Nguyen SA, Meyer TA, Soler ZM, Schlosser RJ. Journal: Int Forum Allergy Rhinol. 2022 Jul;12(7):942-951. doi: 10.1002/alr.22942. Epub 2022 Jan 5. PMID: 34919345