Our Summary
This research paper is about problems with the Eustachian tube, which is a small canal that connects your throat to your middle ear. When this tube isn’t working properly, it can cause a number of symptoms. The paper suggests that it’s important to have clear definitions and ways to diagnose these problems so that patients can get the right treatment. At the moment, there isn’t a widely agreed upon way to diagnose Eustachian tube dysfunction, but the paper puts forward some suggestions.
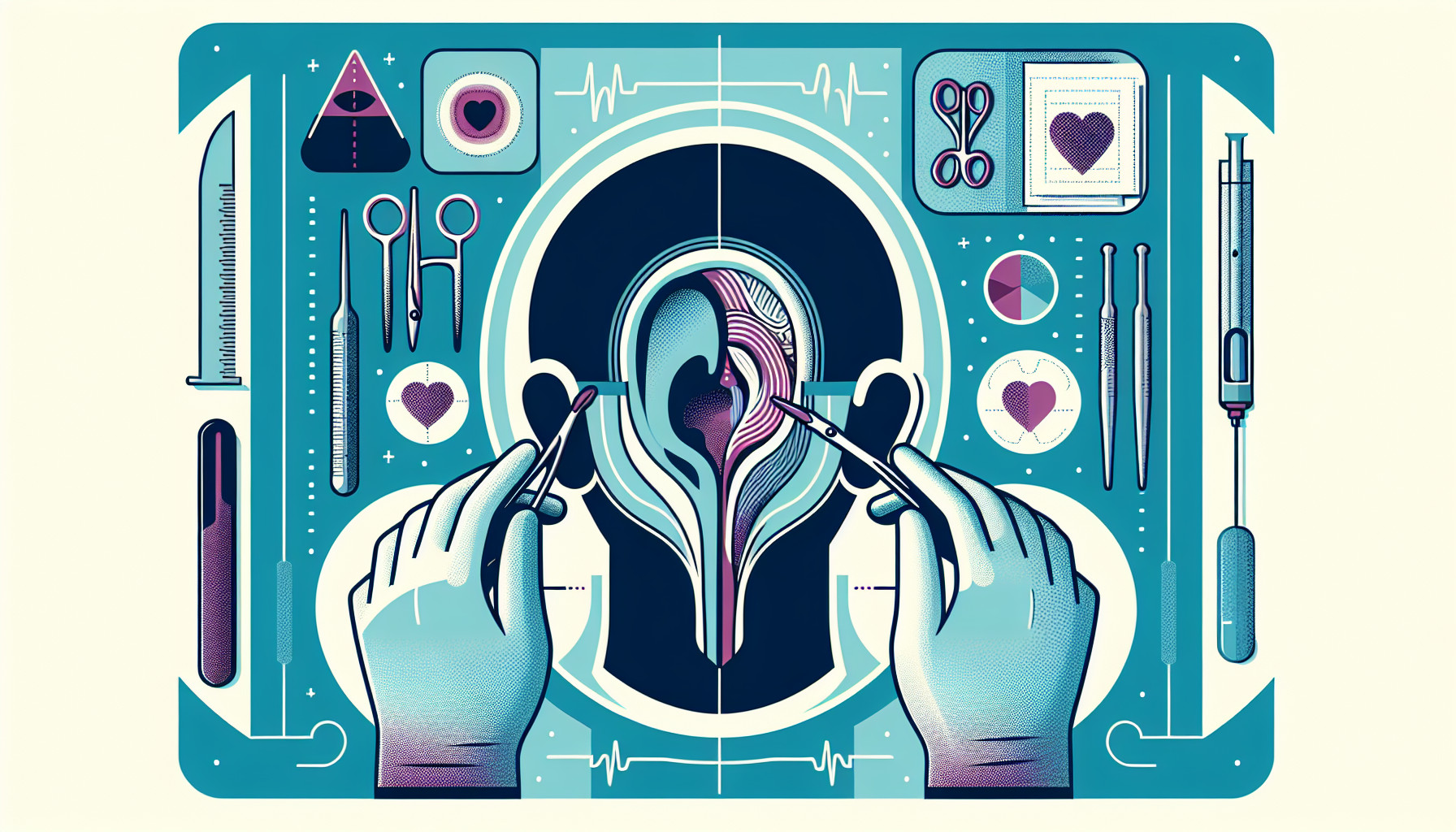
The paper also discusses a diagnostic tool called Tubomanometry, which is used to assess how well the Eustachian tube is functioning, and a treatment method which involves inflating a small balloon inside the Eustachian tube. This can help to improve its function and relieve symptoms in patients.
FAQs
- What is Eustachian tube dysfunction and what are its symptoms?
- What is tubomanometry and how does it help in diagnosing Eustachian tube dysfunction?
- How does balloon dilation of the Eustachian tube help in treating Eustachian tube dysfunction?
Doctor’s Tip
One helpful tip a doctor might tell a patient about ear tube surgery is to ensure they follow all pre-operative instructions provided by their healthcare provider, such as fasting before the procedure and avoiding certain medications. It is also important to have a discussion with the doctor about any concerns or questions they may have before the surgery. After the surgery, the patient should follow all post-operative care instructions, including keeping the ears dry and avoiding activities that could increase the risk of infection. Regular follow-up appointments with the doctor are also important to monitor the healing process and ensure the ear tubes are functioning properly.
Suitable For
Patients who may be recommended ear tube surgery typically have chronic ear infections, frequent middle ear fluid build-up, or Eustachian tube dysfunction that has not improved with other treatments. These patients may experience symptoms such as hearing loss, ear pain, pressure or fullness in the ear, or recurrent ear infections. Ear tube surgery, also known as tympanostomy tube insertion, involves placing small tubes in the eardrum to help ventilate the middle ear and prevent fluid build-up. This surgery is often recommended for children with chronic ear infections or fluid build-up, as well as adults with persistent Eustachian tube dysfunction.
Timeline
Before ear tube surgery:
- Patient may experience frequent ear infections or fluid buildup in the middle ear
- Patient may have difficulty hearing or experience ear pain
- Patient may have trouble with balance or feel pressure in the ear
- Patient may be referred to an ear, nose, and throat specialist for evaluation
After ear tube surgery:
- Patient typically experiences immediate relief from ear pain and pressure
- Patient may have some mild discomfort or drainage from the ear for a few days after surgery
- Patient may notice improved hearing and balance
- Patient may need to follow up with their doctor for a check-up and to monitor the tubes
- Patient may have a reduced risk of future ear infections or fluid buildup in the middle ear
What to Ask Your Doctor
- What are the potential risks and benefits of ear tube surgery?
- How will the surgery be performed and what can I expect during the procedure?
- How long will it take to recover from ear tube surgery?
- Will I need to make any lifestyle or dietary changes after the surgery?
- What follow-up care or appointments will be necessary after ear tube surgery?
- Are there any alternative treatments or therapies for my Eustachian tube dysfunction?
- What are the success rates of ear tube surgery for patients with similar conditions?
- How long do ear tubes typically stay in place and will they need to be replaced in the future?
- Are there any potential complications or long-term effects associated with ear tube surgery?
- Can you provide me with more information about tubomanometry and balloon dilation as diagnostic and treatment options for Eustachian tube dysfunction?
Reference
Authors: Holm NH, Møller MN, Larsen PL, Wanscher JH, Glad H, Gaihede M, Ovesen T. Journal: Ugeskr Laeger. 2019 Jan 14;181(3):V03180209. PMID: 30686280