Our Summary
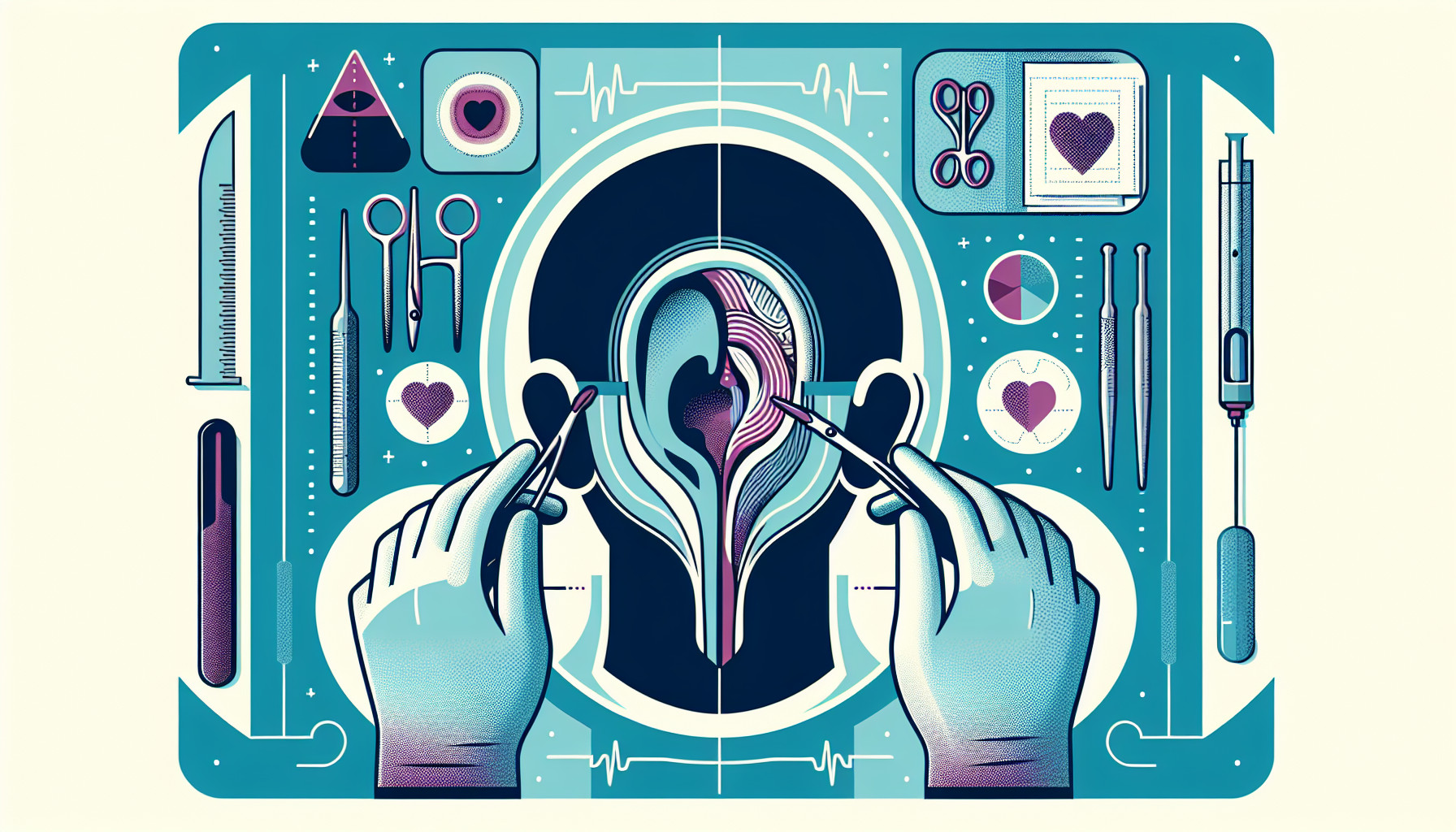
This study looked at the effectiveness of a specific type of ear surgery, Eustachian tube balloon dilation (ETBD), in addition to another common ear procedure, tympanoplasty, in patients with chronic middle ear inflammation and Eustachian tube dysfunction.
The researchers randomly assigned patients to either receive just the tympanoplasty, or to have the ETBD procedure added on.
They then looked at a few things to measure the success of the surgery: changes in the Eustachian Tube Score (ETS), which is a measure of how well the Eustachian tube is functioning, improvements in hearing, and patients’ own experiences of their Eustachian tube functioning.
The results showed that adding the ETBD procedure to the tympanoplasty didn’t make a significant difference in any of these measures. The researchers concluded that ETBD should not be routinely added to tympanoplasty for patients with this condition. They suggested that larger studies could provide more information about when ETBD might be helpful.
FAQs
- What is the purpose of the Eustachian tube balloon dilation (ETBD) and tympanoplasty procedures?
- How were the success of the surgeries measured in this study?
- Did the study find any significant benefits to adding the ETBD procedure to the tympanoplasty?
Doctor’s Tip
A doctor might tell a patient undergoing ear tube surgery to follow post-operative care instructions carefully, including keeping the ear dry and avoiding activities that could introduce water into the ear canal. They may also advise the patient to attend follow-up appointments to monitor healing and ensure the ear tubes are functioning properly. Additionally, the doctor may recommend using ear plugs or cotton balls to protect the ear during activities such as swimming or bathing.
Suitable For
Patients who are typically recommended ear tube surgery are those who have chronic middle ear inflammation and Eustachian tube dysfunction. These patients may experience symptoms such as frequent ear infections, hearing loss, pressure or pain in the ear, and fluid buildup in the middle ear. Ear tube surgery is often recommended for patients who have not responded to other treatments such as antibiotics or decongestants.
Timeline
Before ear tube surgery:
- Patient experiences chronic middle ear inflammation and Eustachian tube dysfunction.
- Patient undergoes evaluation by an ear, nose, and throat specialist to determine the need for surgery.
- Patient may try other treatments such as antibiotics or ear drops before surgery is recommended.
- Patient is informed about the risks and benefits of ear tube surgery and gives consent for the procedure.
After ear tube surgery:
- Patient undergoes the procedure, which typically takes about 15-20 minutes and is done under general anesthesia.
- Patient may experience some discomfort or temporary hearing loss immediately after surgery.
- Patient is typically able to go home the same day as the procedure.
- Patient may need to follow up with their doctor for post-operative care, including keeping the ears dry and using ear drops as prescribed.
- Patient’s symptoms of ear infections, hearing loss, and ear pain should improve following surgery.
- Patient may need to have the tubes removed at a later date, depending on the type of tubes used and how well they are functioning.
What to Ask Your Doctor
What is the purpose of ear tube surgery (ETBD) in addition to tympanoplasty for chronic middle ear inflammation and Eustachian tube dysfunction?
How will the ETBD procedure be performed and what are the potential risks and complications associated with it?
What are the expected outcomes of adding ETBD to tympanoplasty in terms of improving Eustachian tube function, hearing, and overall quality of life?
Are there any alternative treatment options available for my condition that do not involve surgery?
How long is the recovery period expected to be after undergoing both procedures, and what can I do to promote healing and prevent complications?
Will I need follow-up appointments or additional treatments after the surgery, and what signs or symptoms should I watch for that may indicate a need for further medical attention?
Are there any lifestyle changes or precautions I should take after the surgery to protect my ears and prevent future ear problems?
Can you provide me with information about the success rates of ETBD in combination with tympanoplasty for patients with similar conditions to mine?
Are there any specific criteria or factors that would make me a good candidate for adding ETBD to my tympanoplasty procedure?
Are there any ongoing research studies or clinical trials investigating the effectiveness of ETBD for chronic middle ear inflammation and Eustachian tube dysfunction that I may be eligible to participate in?
Reference
Authors: Gey A, Honeder C, Reiber J, Honigmann R, Zirkler J, Wienke A, Rahne T, Plontke SK. Journal: JAMA Otolaryngol Head Neck Surg. 2025 Jul 1;151(7):675-683. doi: 10.1001/jamaoto.2025.0904. PMID: 40372749