Our Summary
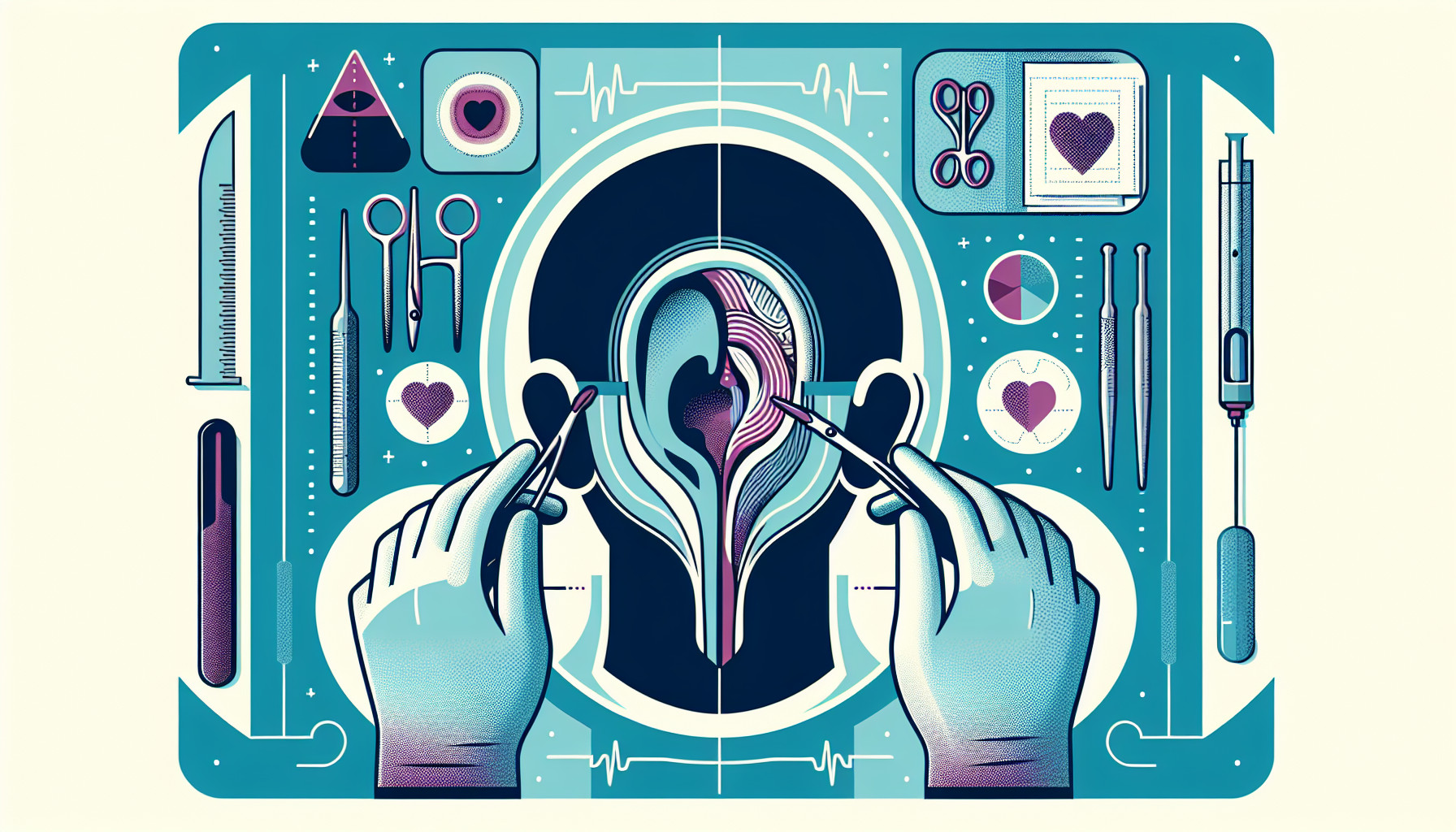
This research paper reviews a surgical procedure called Eustachian tube dilation, specifically balloon dilation Eustachian tuboplasty (BDET), which is used to treat a condition called obstructive Eustachian tube dysfunction. This is a controversial procedure as there currently isn’t a reliable way to diagnose this condition.
However, the paper reveals that in the last two years, two significant trials have shown that BDET can significantly improve symptoms of the condition. This is measured by an improvement in the patient’s ETDQ-7 scores (a tool used to assess symptoms) and a change in abnormal ear-drum behaviour (from type B or C tympanogram to type A tympanogram).
The paper suggests that people who could benefit from BDET are those who have experienced a feeling of fullness in the ear for more than 12 weeks, have a type B or C tympanogram, have an ETDQ-7 mean score of more than 2, and have not seen improvement from other treatments such as the Valsalva maneuver (a method of clearing the ears), nasal steroids for four weeks, or oral steroids for one week.
FAQs
- What is balloon dilation Eustachian tuboplasty (BDET) and what is it used to treat?
- What improvements can be seen in patients who undergo BDET surgery?
- Who are the ideal candidates for BDET surgery according to the paper?
Doctor’s Tip
Additionally, the paper emphasizes the importance of discussing the risks and benefits of BDET with your doctor before proceeding with the procedure. It is important to understand that like any surgery, there are potential risks involved such as infection, bleeding, and damage to surrounding structures. Your doctor may also provide advice on how to care for your ears post-surgery to ensure proper healing and minimize the risk of complications.
Overall, the paper highlights the potential benefits of BDET for patients with obstructive Eustachian tube dysfunction and encourages individuals to have an open and informed discussion with their healthcare provider to determine if this procedure is the right option for them.
Suitable For
Additionally, patients who have recurrent ear infections, hearing loss, or balance issues due to Eustachian tube dysfunction may also be recommended for ear tube surgery. It is important for patients to consult with an ENT specialist to determine if they are a candidate for ear tube surgery and to discuss the potential risks and benefits of the procedure.
Timeline
- Before surgery:
- Patient experiences symptoms of obstructive Eustachian tube dysfunction, such as ear fullness, pressure, or pain for more than 12 weeks.
- Patient undergoes diagnostic tests, such as tympanometry and ETDQ-7 questionnaire, to confirm the diagnosis.
- Patient tries conservative treatments, such as Valsalva maneuver, nasal steroids, or oral steroids, without improvement.
- Patient meets criteria for BDET, including type B or C tympanogram and ETDQ-7 mean score of more than 2.
- After surgery:
- Patient undergoes BDET procedure, which involves balloon dilation of the Eustachian tube to improve function.
- Patient experiences improvement in symptoms, as measured by a decrease in ETDQ-7 scores and a change in tympanogram to type A.
- Patient may have follow-up appointments to monitor their progress and assess the effectiveness of the procedure.
- Patient may experience long-term relief from symptoms and improved quality of life following BDET surgery.
What to Ask Your Doctor
- What is the success rate of balloon dilation Eustachian tuboplasty (BDET) for treating obstructive Eustachian tube dysfunction?
- What are the potential risks and complications associated with BDET surgery?
- How long is the recovery time after BDET surgery, and what can I expect during the recovery process?
- Will I need to follow any specific post-operative care instructions after BDET surgery?
- How long do the effects of BDET surgery typically last?
- Are there any alternative treatments for obstructive Eustachian tube dysfunction that I should consider before opting for BDET surgery?
- How many BDET procedures have you performed, and what is your experience with this surgery?
- Can you explain the diagnostic criteria for obstructive Eustachian tube dysfunction and how it is determined that BDET surgery is the appropriate treatment for me?
- What is the expected outcome of BDET surgery in terms of symptom improvement and long-term management of obstructive Eustachian tube dysfunction?
- Are there any specific lifestyle changes or precautions I should take after undergoing BDET surgery to prevent recurrence of symptoms?
Reference
Authors: Siow JK, Tan JL. Journal: Curr Opin Otolaryngol Head Neck Surg. 2020 Feb;28(1):31-35. doi: 10.1097/MOO.0000000000000601. PMID: 31789929